Less than a year ago, this was decried as a conspiracy theory cooked up by paranoid tinfoil hatters. Now, the World Health Organization is openly discussing policies of MANDATORY injections. And to clarify, all of these gene-replacement “vaccines” are still considered experimental. They are authorized for emergency measures, but are not actually approved.
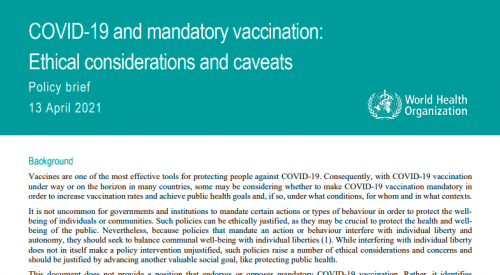
WHO Paper On MANDATORY Vaccination April 13, 2021 (Original)
WHO Paper On MANDATORY Vaccination April 13, 2021 (Copy)
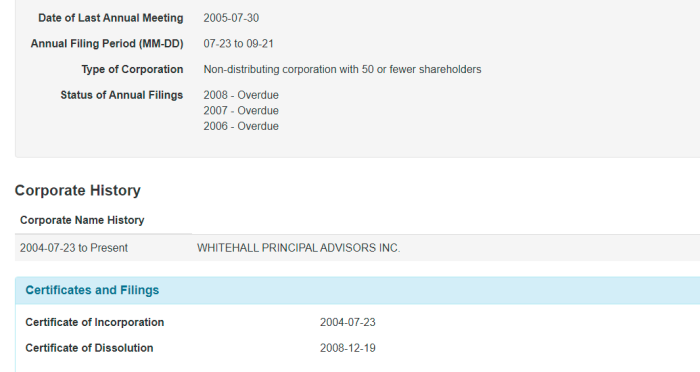
Section 30.1 Canada Food & Drug Act
September 2020 Interim Order From Patty Hajdu
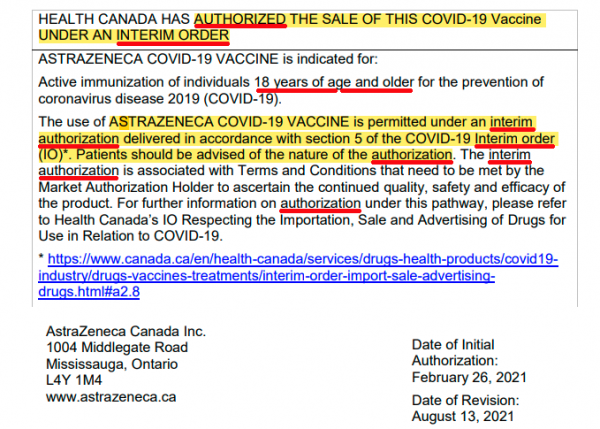
https://covid-vaccine.canada.ca/info/pdf/astrazeneca-covid-19-vaccine-pm-en.pdf
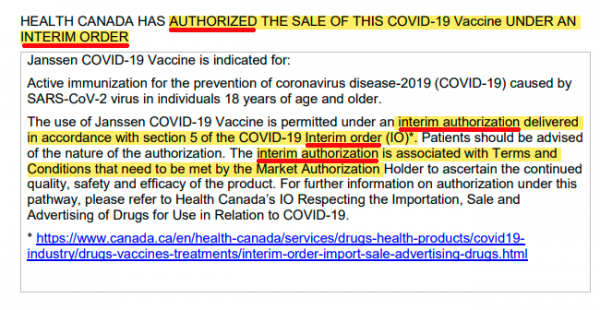
https://covid-vaccine.canada.ca/info/pdf/janssen-covid-19-vaccine-pm-en.pdf
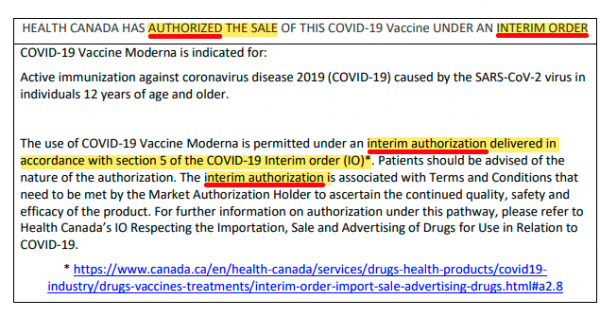
https://covid-vaccine.canada.ca/info/pdf/covid-19-vaccine-moderna-pm-en.pdf
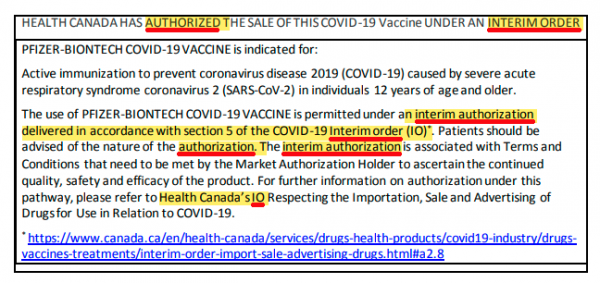
https://covid-vaccine.canada.ca/info/pdf/pfizer-biontech-covid-19-vaccine-pm1-en.pdf
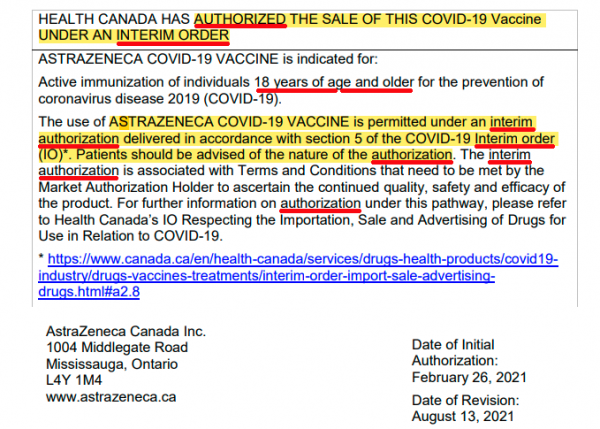
Testing Product Insert AstraZeneca Interim Authorization
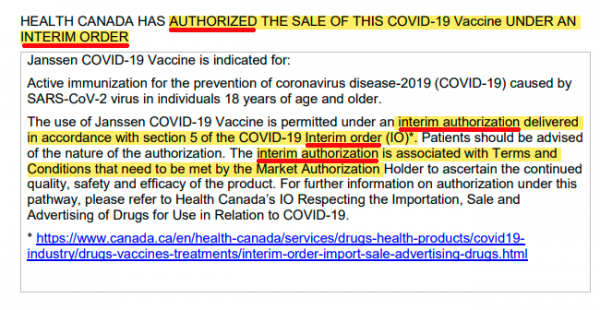
Testing Product Insert Janssen Interim Authorization
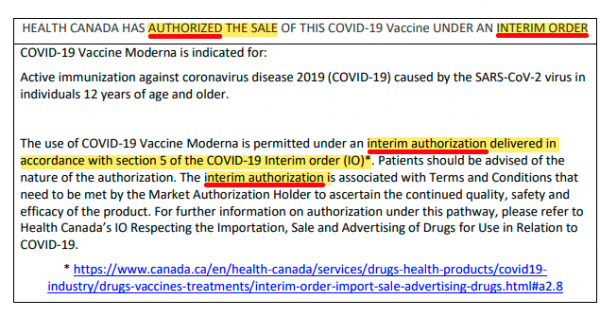
Testing Product Insert Moderna Interim Authorization
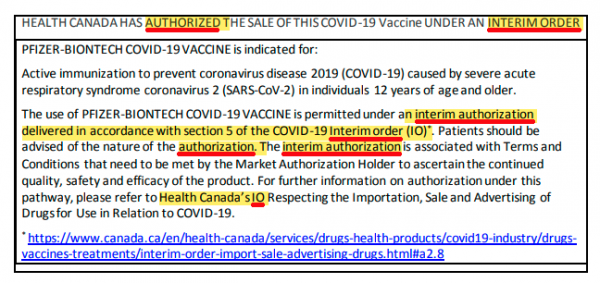
Testing Product Insert Pfizer Interim Authorization
Before going any further, it is time to distinguish between 2 completely different ways medical devices and substances can be advanced.
(a) Approved: Health Canada has fully reviewed all the testing, and steps have been done, with the final determination that it can be used for the general population
(b) Interim Authorization: deemed to be “worth the risk” under the circumstances, doesn’t have to be fully tested. Allowed under Section 30.1 of the Canada Food & Drug Act. Commonly referred to as an emergency use authorization.
To be approved means that this thing has been rigorously tested, and has passed all safety measures, and that it has rigorously been examined. This is not what happened here. Instead, these “vaccines” were given interim authorization, because the Government has decided that it’s worth releasing it to the general public, and finishing the testing later. This is allowed under Section 30.1 of the Canada Food & Drug Act, and an Interim Order was signed by Patty Hajdu.
Think this is an exaggeration? Take a look at the paperwork available from Health Canada. Not once do they refer to them as approved. Instead, they are “authorized under an Interim Order”. These are not the same thing, and cannot be used interchangeably. Now, let’s get to the WHO paper.
Vaccines are one of the most effective tools for protecting people against COVID-19. Consequently, with COVID-19 vaccination under way or on the horizon in many countries, some may be considering whether to make COVID-19 vaccination mandatory in order to increase vaccination rates and achieve public health goals and, if so, under what conditions, for whom and in what contexts
Right off the bat, there is no semblance of neutrality. The World Health Organization starts off with the assumption that these are safe and effective. So legitimate concerns about testing, long term side effects, and the necessity of these “vaccines” is minimized.
It is not uncommon for governments and institutions to mandate certain actions or types of behaviour in order to protect the well-being of individuals or communities. Such policies can be ethically justified, as they may be crucial to protect the health and well-being of the public. Nevertheless, because policies that mandate an action or behaviour interfere with individual liberty and autonomy, they should seek to balance communal well-being with individual liberties. While interfering with individual liberty does not in itself make a policy intervention unjustified, such policies raise a number of ethical considerations and concerns and should be justified by advancing another valuable social goal, like protecting public health.
.
This document does not provide a position that endorses or opposes mandatory COVID-19 vaccination. Rather, it identifies important ethical considerations and caveats that should be explicitly evaluated and discussed through ethical analysis by governments and/or institutional policy-makers who may be considering mandates for COVID-19 vaccination.
Interesting. This paper attempts to take a neutral and academic approach towards the idea of forced vaccinations (or gene replacement therapy). How exactly does someone take a neutral stance on forcing millions, or billions, or people to take experimental drugs? Is this really necessary for safety?
How do you balance: (a) your right to self autonomy and control over your own body, and (b) the doomsday predictions of sociopathic politicians, and corrupt scientists?
1. Necessity and proportionality
Mandatory vaccination should be considered only if it is necessary for, and proportionate to, the achievement of an important public health goal (including socioeconomic goals) identified by a legitimate public health authority. If such a public health goal (e.g., herd immunity, protecting the most vulnerable, protecting the capacity of the acute health care system) can be achieved with less coercive or intrusive policy interventions (e.g., public education), a mandate would not be ethically justified, as achieving public health goals with less restriction of individual liberty and autonomy yields a more favourable risk-benefit ratio.
.
As mandates represent a policy option that interferes with individual liberty and autonomy, they should be considered only if they would increase the prevention of significant risks of morbidity and mortality and/or promote significant and unequivocal public health benefits. If important public health objectives cannot be achieved without a mandate – for instance, if a substantial portion of individuals are able but unwilling to be vaccinated and this is likely to result in significant risks of harm – their concerns should be addressed, proactively if possible. If addressing such concerns is ineffective and those concerns remain a barrier to achievement of public health objectives and/or if low vaccination rates in the absence of a mandate put others at significant risk of serious harm, a mandate may be considered “necessary” to achieve public health objectives. In this case, those proposing the mandate should communicate the reasons for the mandate to the affected communities through effective channels and find ways to implement the mandate such that it accommodates the reasonable concerns of communities. Individual liberties should not be challenged for longer than necessary. Policy-makers should therefore frequently re-evaluate the mandate to ensure it remains necessary and proportionate to achieve public health goals. In addition, the necessity of a mandate to achieve public health goals should be evaluated in the context of the possibility that repeated vaccinations may be required as the virus evolves, as this may challenge the possibility of a mandate to realistically achieve intended public health objectives.
Our “leaders” rely on computer modelling and data manipulation in order to drive these predictions. Therefore, the case of necessity can always be skewed. Liberties should not be challenged longer than necessary, yet the only way to achieve it — at some point — is to take experimental drugs.
Not only should we consider mandating these “vaccines”, we should also consider if more and more will be needed to deal with mutations of it.
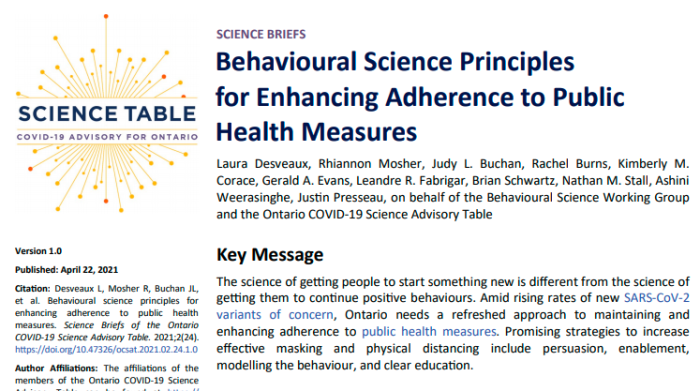
There’s little to no concern about the long term effects of these “vaccines”. In fact, the authors parrot the talking points that they are safe and effective. The only issue seems to be about making it required if they cannot “educate” the public in sufficient numbers.
2. Sufficient evidence of vaccine safety
.
Data should be available that demonstrate the vaccine being mandated has been found to be safe in the populations for whom the vaccine is to be made mandatory. When safety data are lacking or when they suggest the risks associated with vaccination outweigh the risks of harm without the vaccine, the mandate would not be ethically justified, particularly without allowing for reasonable exceptions (e.g., medical contraindications). Policy-makers should consider specifically whether vaccines authorized for emergency or conditional use meet an evidentiary threshold for safety sufficient for a mandate. In the absence of sufficient evidence of safety, there would be no guarantee that mandating vaccination would achieve the goal of protecting public health. Furthermore, coercive exposure of populations to a potentially harmful product would violate the ethical obligation to protect the public from unnecessary harm when the harm the product might cause outweighs the degree of harm that might exist without the product. Even when the vaccine is considered sufficiently safe, mandatory vaccination should be implemented with no-fault compensation schemes to address any vaccine-related harm that might occur. This is important, as it would be unfair to require people who experience vaccine-related harm to seek legal remedy from harm resulting from a mandatory intervention. Such compensation would depend on countries’ health systems, including the extent of universal health coverage and how they address harm from vaccines that are not fully licensed (e.g., vaccines authorized for emergency or conditional use).
.
3. Sufficient evidence of vaccine efficacy and effectiveness
.
Data on efficacy and effectiveness should be available that show the vaccine is efficacious in the population for whom vaccination is to be mandated and that the vaccine is an effective means of achieving an important public health goal. For instance, if mandatory vaccination is considered necessary to interrupt transmission chains and prevent harm to others, there should be sufficient evidence that the vaccine is efficacious in preventing serious infection and/or transmission. Alternatively, if a mandate is considered necessary to prevent hospitalization and protect the capacity of the acute health care system, there should be sufficient evidence that the vaccine is efficacious in reducing hospitalization. Policy-makers should carefully consider whether vaccines authorized for emergency or conditional use meet evidentiary thresholds for efficacy and effectiveness sufficient for a mandate.
Here we get to the heart of it. The World Health Organization mentions that policy makers might consider a mandate, even if these gene replacement “vaccines” have only emergency or conditional authorization. As mentioned earlier, that is what status the chemicals in Canada have.
Vaccine compensation programs should be established, but that leaves out a key detail. It’s not the drug manufacturers who would be paying for such injuries. It would be funded by the public. Privatized profits, socialized losses.
There’s also the interesting question: if an experimental or emergency use “vaccine” is taken, who actually is responsible for it?
Mandatory COVID-19 vaccination in context
.
Authorized COVID-19 vaccines have been shown to be safe and efficacious in preventing severe disease and death, and it is clear that vaccine supply will continue to increase globally, albeit inequitably. That being said, the nature of the COVID-19 pandemic and evidence on vaccine safety, efficacy, and effectiveness continue to evolve (including with respect to variants of concern). Consequently, the six considerations identified above are described generally so that they can be applied at any point in time and in any context. For illustrative purposes, we now turn our attention to the application of these ethical considerations in three settings for which mandatory vaccination is commonly discussed: for the general public, in schools, and for health workers.
Within this paragraph, it’s stated that authorized vaccines (again, not approved), are safe and efficacious. Then, it immediately claims this will continue to evolve. In other words, these “safety” guarantees are worth nothing.
Conclusions
Vaccines are effective for protecting people from COVID-19. Governments and/or institutional policy-makers should use arguments to encourage voluntary vaccination against COVID-19 before contemplating mandatory vaccination. Efforts should be made to demonstrate the benefit and safety of vaccines for the greatest possible acceptance of vaccination. Stricter regulatory measures should be considered only if these means are not successful. A number of ethical considerations and caveats should be explicitly discussed and addressed through ethical analysis when considering whether mandatory COVID-19 vaccination is an ethically justifiable policy option. Similar to other public health policies, decisions about mandatory vaccination should be supported by the best available evidence and should be made by legitimate public health authorities in a manner that is transparent, fair, non-discriminatory, and involves the input of affected parties.
WHO Paper On MANDATORY Vaccination April 13, 2021 (Original)
WHO Paper On MANDATORY Vaccination April 13, 2021 (Copy)
Use arguments first. Mandate only if that doesn’t work. In other words, if we can’t persuade people to take it willingly, then consider forcing them. Funny how “involves the input of affected parties” gets in there. If these are mandated, then of course input is removed.
Don’t you love it when academic debate what our human rights should be, and what bodily autonomy we should have?
References
1. Nuffield Council on Bioethics. Public health: Ethical issues. London: Nuffield Council on Bioethics; 2007
(https://www.nuffieldbioethics.org/assets/pdfs/Public-health-ethical-issues.pdf).
2. Gravagna K, Becker A, Valeris-Chacin R, Mohammed I, Tambe S, Awan FA et al. Global assessment of national
mandatory vaccination policies and consequences of non-compliance. Vaccine. 2020;38:7865–73.
3. Colgrove J, Bayer R. Manifold restraints: Liberty, public health, and the legacy of Jacobson v Massachusetts. Am J Public
Health. 2005;95:571–6.
4. World Health Organization. COVID-19 virtual press conference 7 December 2020
(https://www.who.int/publications/m/item/covid-19-virtual-press-conference-transcript—7-december-2020).
5. World Health Organization. Interim position paper: Considerations regarding proof of COVID-19 vaccination for
international travellers. Geneva: World Health Organization; 2021 (https://www.who.int/news-room/articles-detail/interim-position-paper-considerations-regarding-proof-of-covid-19-vaccination-for-international-travellers).
6. Walkinshaw E. Mandatory vaccinations: The international landscape. Can Med Assoc J. 2011;183:e1167–8.
7. Gostin LO, Salmon DA, Larson HJ. Mandating COVID-19 vaccines. JAMA. 2020;325:532–3.
8. Halabi S, Heinrich A, Omer S. No-fault compensation for vaccine injury – The other side of equitable access to Covid-19
vaccines. N Engl J Med. 2020;383:e125.
9. Schwartz JL. Evaluating and deploying Covid-19 vaccines – The importance of transparency, scientific integrity, and
public trust. N Engl J Med. 2020;383:1703–5.
10. Shetty P. Experts concerned about vaccination backlash. Lancet. 2020;375:970–1.
11. Giubilini A. Chapter 3, Vaccination policies and the principle of least restrictive alternative: An intervention ladder. In
Giubilini A, The ethics of vaccination. Cham (CH): Palgrave Pivot; 2019.
12. Goldenberg M. Vaccine hesitancy: Public trust, expertise, and the war on science. Pittsburgh, PA: University of Pittsburgh
Press. 2021.
13. Opel DJ, Lo B, Peek ME. Addressing mistrust about COVID-19 vaccines among patients of color. Ann Intern Med.
2021;M21-0055. doi: 10.7326/M21-0055.
14. Colgrove J. Immunization and ethics: Beneficence, coercion, public health, and the state. In: Mastroianni AC, Kahn JP,
Kass NE, editors. The Oxford handbook of public health ethics, New York City (NY): Oxford University Press; 2020:435–
44.
15. Sutton EJ, Upshur REG. Are there different spheres of conscience? J Eval Clin Pract. 2010;16:338–43.
16. Harris J, Holm S. Is there a moral obligation not to infect others? BMJ. 1995;311:1215–7.
17. Gruben V, Siemieniuk RA, McGeer A. Health care workers, mandatory influenza vaccination policies and the law. Can
Med Assoc J. 2014;186:1076–80.
18. Krystal JH. Responding to the hidden pandemic for healthcare workers: Stress. Nat Med. 2020;26:639.
19. Van Buynder PG, Konrad S, Kersteins F, Preston E, Brown PD, Keen D, et al. Healthcare worker influenza immunization
vaccinate or mask policy: Strategies for cost effective implementation and subsequent reductions in staff absenteeism due
to illness. Vaccine. 2015;33:625–8.
20. Caplan A, Shah NR. Managing the human toll caused by seasonal influenza: New York State’s mandate to vaccinate or
mask. JAMA. 2013;310:1797–8.
21. World Health Organization. Mask use in the context of COVID-19 – Interim guidance. Geneva: World Health
Organization; 2020. (https://www.who.int/publications/i/item/advice-on-the-use-of-masks-in-the-community-during�home-care-and-in-healthcare-settings-in-the-context-of-the-novel-coronavirus-(2019-ncov)-outbreak)
Like this:
Like Loading...