1. Other Articles On CV “Planned-emic”
The rest of the series is here. Many lies, lobbying, conflicts of interest, and various globalist agendas operating behind the scenes, obscuring the vile agenda called the “Great Reset“. The Gates Foundation finances: the WHO, the US CDC, GAVI, ID2020, John Hopkins University, Imperial College London, the Pirbright Institute, the BBC, and individual pharmaceutical companies. Also: there is little to no science behind what our officials are doing; they promote degenerate behaviour; and the International Health Regulations are legally binding. See here, here, and here. The media is paid off, and our democracy compromised, shown: here, here, here, and here.
2. Important Links
https://apps.who.int/iris/handle/10665/331693
April 6 WHO Guidance On Masks
https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/when-and-how-to-use-masks
June 5 WHO Guidance On Masks
WHO On Forcing Masks On Children
August 21 WHO Guidance For Masks On Children
WHO On Masks: December 1 Update
December 1 WHO Guidance On Masks
Note: for more context for this article, check Part 37A. That refers to the April 6 and June 5 guidelines handed down by the World Health Organization. In short, they still aren’t checking for logical consistency.
3. Quotes From December 1 Guidance

BC’s tyrant-in-chief, Bonnie Henry, has said that she has no time for people who think that masks cause health problems, or reduce their freedom. This flies in the face on WHO guidelines, and even her own dictates. Henry gaslights people, despite there being no science behind limiting group sizes, or most things she says.
[Page 1]
This document, which is an update of the guidance published on 5 June 2020, includes new scientific evidence relevant to the use of masks for reducing the spread of SARS-CoV-2, thevirus that causes COVID-19, and practical considerations. It contains updated evidence and guidance on the following:
In case this isn’t obvious, this is suppose to reflect changes and more information coming out. Supposedly the evidence and knowledge evolves, as the situation requires it.
[Page 1]
The World Health Organization (WHO) advises the use of masks as part of a comprehensive package of prevention and control measures to limit the spread of SARS-CoV-2, the virus that causes COVID-19. A mask alone, even when it is used correctly, is insufficient to provide adequate protection or source control. Other infection prevention and control (IPC) measures include hand hygiene, physical distancing of at least 1 metre, avoidance of touching one’s face, respiratory etiquette, adequate ventilation in indoor settings, testing, contacttracing, quarantine and isolation. Together these measures are critical to prevent human-to-human transmission of SARS-CoV-2.
WHO still recommends face masks. Keep that point in mind. Also, it’s been mentioned before that WHO suggests people being 1m apart. There is no reference to 2m on their site.
[Page 3]
The presence of viral RNA is not the same as replication- and infection-competent (viable) virus that could be transmissible and capable of sufficient inoculum to initiate invasive infection. A limited number of studies have isolated viable SARS-CoV-2 from air samples in the vicinity of COVID-19 patients (20, 21).
This pretty much blows the whole PCR test out of the water. Simply having traces present doesn’t you are infected.
[Page 3]
High quality research is required to address the knowledge gaps related to modes of transmission, infectious dose and settings in which transmission can be amplified. Currently, studies are underway to better understand the conditions in which aerosol transmission or superspreading events may occur.
.
Current evidence suggests that people infected with SARSCoV-2 can transmit the virus whether they have symptoms or not. However, data from viral shedding studies suggest that infected individuals have highest viral loads just before or around the time they develop symptoms and during the first 5-7 days of illness (12). Among symptomatic patients, the duration of infectious virus shedding has been estimated at 8 days from the onset of symptoms (22-24) for patients with mild disease, and longer for severely ill patients (12). The period of infectiousness is shorter than the duration of detectable RNA shedding, which can last many weeks (17).
Research is still needed? That’s a pretty big thing to admit, since supposedly the vaccines are here, and ready to go. It seems that we won’t need it after all.
As for the claim that asymptomatic transmission is possible, that is likely a response to this bombshell dropped on June 8, 2020. WHO admitted asymptomatic transmission was very rare, but there was quite predictably a lot of anger and confusion over that. Maria Van Kerkhove spent the next day backtracking. See below.
Back in June, the WHO thought that as much as 41% of the global population could be infected, which is over 3 billion people. In reality, they have no idea.
[Page 5]
Evidence on universal masking in health care settings
.
In areas where there is community transmission or large-scale outbreaks of COVID-19, universal masking has been adopted in many hospitals to reduce the potential of transmission by health workers to patients, to other staff and anyone else entering the facility (50).
.
Two studies found that implementation of a universal masking policy in hospital systems was associated with
decreased risk of healthcare-acquired SARS-CoV-2 infection. However, these studies had serious limitations: both were before-after studies describing a single example of a phenomenon before and after an event of interest, with no concurrent control group, and other infection control measures were not controlled for (51, 52). In addition, observed decreases in health worker infections occurred too quickly to be attributable to the universal masking policy.
Universal masking seems to be the case in hospital settings. However, some of the scientific research supporting it has serious limitations.
[Page 6]
Fabric masks are not regulated as protective masks or part of the PPE directive. They vary in quality and are not subject to mandatory testing or common standards and as such are not considered an appropriate alternative to medical masks for protection of health workers. One study that evaluated the use of cloth masks in a health care facility found that health care workers using 2 ply cotton cloth masks (a type of fabric mask) were at increased risk of influenza-like illness compared with those who wore medical masks (72).
Interesting. Using cloth masks actually increased the risk of influenza like illnesses. But just wear a mask anyway.
[Page 8]
Evidence on the protective effect of mask use in community settings
.
At present there is only limited and inconsistent scientific evidence to support the effectiveness of masking of healthy people in the community to prevent infection with respiratory viruses, including SARS-CoV-2 (75). A large randomized community-based trial in which 4862 healthy participants were divided into a group wearing medical/surgical masks and a control group found no difference in infection with SARS-CoV-2 (76). A recent systematic review found nine trials (of which eight were cluster-randomized controlled trials in which clusters of people, versus individuals, were randomized) comparing medical/surgical masks versus no masks to prevent the spread of viral respiratory illness. Two trials were with healthcare workers and seven in the community. The review concluded that wearing a mask may make little or no difference to the prevention of influenza-like illness
Even a good chunk of their own research concluded there was little to no benefit to forcing masks on the general population.
[Page 8]
Guidance
The WHO COVID-19 IPC GDG considered all available evidence on the use of masks by the general public including
effectiveness, level of certainty and other potential benefits and harms, with respect to transmission scenarios, indoor versus outdoor settings, physical distancing and ventilation. Despite the limited evidence of protective efficacy of mask wearing in community settings, in addition to all other recommended preventive measures, the GDG advised mask wearing in the following settings:
WHO recommends mask wearing in many situations, despite limited evidence it actually works. Again, all of this is from their own report.
[Page 10]
The potential disadvantages of mask use by healthy people in the general public include:
• headache and/or breathing difficulties, depending on type of mask used (55);
• development of facial skin lesions, irritant dermatitis or worsening acne, when used frequently for long hours (58, 59, 127);
• difficulty with communicating clearly, especially for persons who are deaf or have poor hearing or use lipreading (128, 129);
• discomfort (44, 55, 59)
• a false sense of security leading to potentially lower adherence to other critical preventive measures such as physical distancing and hand hygiene (105);
• poor compliance with mask wearing, in particular by young children (111, 130-132);
• waste management issues; improper mask disposal leading to increased litter in public places andenvironmental hazards (133);
• disadvantages for or difficulty wearing masks, especially for children, developmentally challenged persons, those with mental illness, persons with cognitive impairment, those with asthma or chronic respiratory or breathing problems, those who have had facial trauma or recent oral maxillofacial surgery and those living in hot and humid environments (55, 130).
This is essentially a cut-and-paste from earlier guidance. Note: even though breathing problems are specifically listed, Bonnie Henry has no time for such people.
[Page 11]
Mask use during physical activity Evidence
.
There are limited studies on the benefits and harms of wearing medical masks, respirators and non-medical masks while exercising. Several studies have demonstrated statistically significant deleterious effects on various cardiopulmonary physiologic parameters during mild to moderate exercise in healthy subjects and in those with underlying respiratory diseases (134-140). The most significant impacts have been consistently associated with the use of respirators and in persons with underlying obstructive airway pulmonary diseases such as asthma and chronic obstructive pulmonary disease (COPD), especially when the condition is moderate to severe (136). Facial microclimate changes with increased temperature, humidity and perceptions of dyspnoea were also reported in some studies on the use of masks during exercise (134, 141). A recent review found negligeable evidence of negative effects of mask use during exercise but noted concern for individuals with severe cardiopulmonary disease (142).
The World Health Organization discourages the use of masks for people who are exercising. Good to know. However, is must be asked if people were deliberately subjected to this is order to gather data for the research.
[Page 19]
Background
A non-medical mask, also called fabric mask, community mask or face covering, is neither a medical device nor personal protective equipment. Non-medical masks are aimed at the general population, primarily for protecting others from exhaled virus-containing droplets emitted by the mask wearer. They are not regulated by local health authorities or occupational health associations, nor is it required for manufacturers to comply with guidelines established by standards organizations. Non-medical masks may be homemade or manufactured. The essential performance parameters include good breathability, filtration of droplets originating from the wearer, and a snug fit covering the nose and mouth. Exhalation valves on masks are discouraged as they bypass the filtration function of the mask.
Non-medical masks have no real standards for manufacturing.
[Page 19]
Evidence on the effectiveness of non-medical (fabric) masks
.
A number of reviews have been identified on the effectiveness of non-medical masks (151-156). One systematic review (155) identified 12 studies and evaluated study quality. Ten were laboratory studies (157-166), and two reports were from a single randomized trial (72, 167). The majority of studies were conducted before COVID-19 emerged or used laboratory generated particles to assess filtration efficacy. Overall, the reviews concluded that cloth face masks have limited efficacy in combating viral infection transmission.
Sure, there’s limited evidence they actually work. But just wear a mask, any mask, because it’s about community safety.
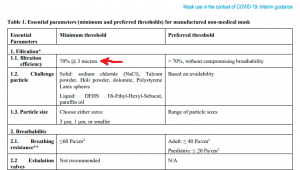
(from page 21): WHO recommends masks be able to filter out 70% or more of particles, at 3 microns or more. That is pretty meaningless since the virus is less then 1/10 that diameter.
4. Thoughts On Latest Guidance
Even giving the World Health Organization every benefit of the doubt, its own reports admit the evidence on mask use is limited and often contradictory. The recommendations are based on politics, not science.
Talking about the “Great Reset” or the depopulation agenda would be nice, but that sort of transparency is most unlikely.
Discover more from Canuck Law
Subscribe to get the latest posts sent to your email.
