Let’s take a look into how the World Health Organization defines cases, and causes of death.
1. Other Articles On CV “Planned-emic”
The rest of the series is here. Many lies, lobbying, conflicts of interest, and various globalist agendas operating behind the scenes, obscuring the vile agenda called the “Great Reset“. The Gates Foundation finances: the WHO, the US CDC, GAVI, ID2020, John Hopkins University, Imperial College London, the Pirbright Institute, the BBC, and individual pharmaceutical companies. Also: there is little to no science behind what our officials are doing; they promote degenerate behaviour; the Australian Department of Health admits the PCR tests don’t work; the US CDC admits testing is heavily flawed; and The International Health Regulations are legally binding. See here, here, and here. The media is paid off, and our democracy compromised, shown: here, here, here, and here.
2. Important Links
January 17, 2020 Testing Guidelines For WHO
March 19, 2020 Testing Guidelines For WHO
September 11, 2020 Testing Guidelines For WHO
September 11, 2020 WHO-2019-nCoV-Antigen_Detection
WHO: January, March, September 2020 Guidelines
WHO’s January 13, 2021 Posting On Test Guidelines
January 31 Global Surveillance For Human Infection
March 20 Global Surveillance For Human Infection
May 10 Global Surveillance For Human Infection
August 7 Global Surveillance For Human Infection
December 16 Global Surveillance For Human Infection
https://www.who.int/classifications/icd/Guidelines_Cause_of_Death_COVID-19.pdf
WHO Guidelines Classification Of Death
WHO Case Definition Guidelines
BCCDC: No Idea Actual Error Rate Of PCR Tests
BC COVID19_SerologyTestingGuidelines (1)
BC COVID19_InterpretingTesting_Results_NAT_PCR
Tricity: Bonnie Henry – False Positives Overwhelming Hospitals
CBC: Bonnie Henry Warning About False Negatives
WHO’s Definition Of “Herd Immunity”
WHO Posting On Herd Immunity Definition
WHO’s Other Definition Of Herd Immunity
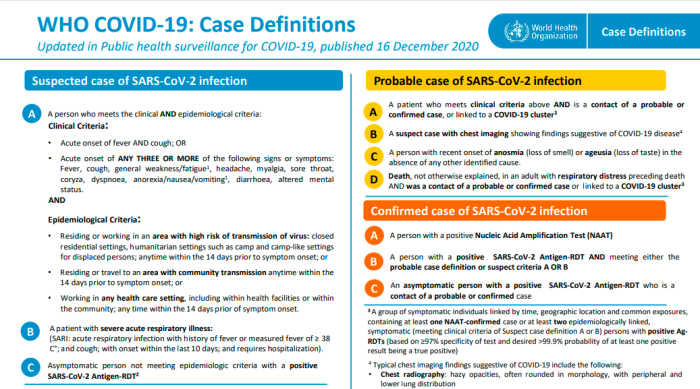
3. Case Definitions Are Quite Subjective
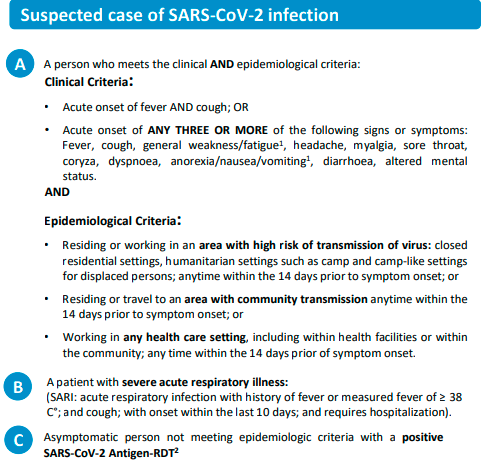
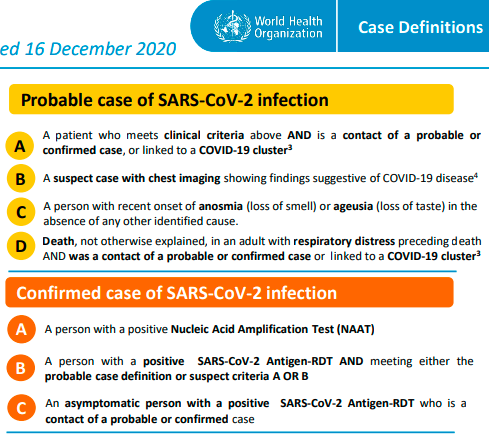
Given the way that the “probable” cases are defined, it’s entirely possible to classify many thousands of people without doing a single test to confirm. Perhaps this is why it’s so vague, in order to generate false positives when needed.
4. Guidelines For Listing Causes Of Death
1. PURPOSE OF THE DOCUMENT
This document describes certification and classification (coding) of deaths related to COVID-19. The primary goal is to identify all deaths due to COVID-19.
.
A simplified section specifically addresses the persons that fill in the medical certificate of cause of death. It should be distributed to certifiers separate from the coding instructions.
2. DEFINITION FOR DEATHS DUE TO COVID-19
A death due to COVID-19 is defined for surveillance purposes as a death resulting from a clinically compatible illness, in a probable or confirmed COVID-19 case, unless there is a clear alternative cause of death that cannot be related to COVID disease (e.g. trauma). There should be no period of complete recovery from COVID-19 between illness and death.
.
A death due to COVID-19 may not be attributed to another disease (e.g. cancer) and should be counted independently of preexisting conditions that are suspected of triggering a severe course of COVID-19.
In fairness this may just be extremely poor wording. However, it appears that the default position is to count deaths in confirmed OR PROBABLE cases if the death is from an illness COMPATIBLE WITH Covid-19 symptoms, and we should downplay PREEXISTING CONDITIONS that may have contributed.
As with the diagnosing of cases, there is no requirement to have a positive test. Speaks volumes about how shady this method is.
Now there is the disclaimer that it should not be counted if there is a clear alternative, but this appears to be just an afterthought.
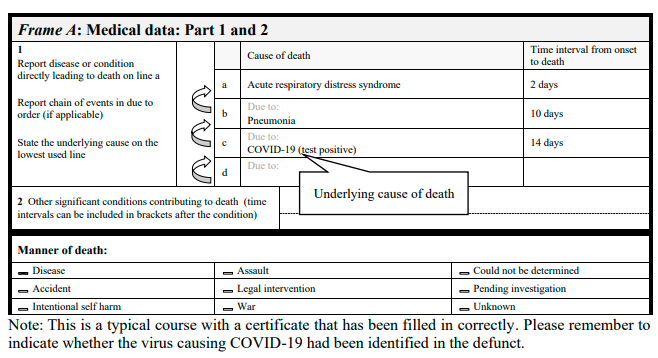
C- CHAIN OF EVENTS
Specification of the causal sequence leading to death in Part 1 of the certificate is important. For example, in cases when COVID-19 causes pneumonia and fatal respiratory distress, both pneumonia and respiratory distress should be included, along with COVID-19, in Part 1. Certifiers should include as much detail as possible based on their knowledge of the case, as from medical records, or about laboratory testing.
<
p style=”padding: 2px 6px 4px 6px; color: #555555; background-color: #eeeeee; border: #dddddd 2px solid;”>
D- COMORBIDITIES
There is increasing evidence that people with existing chronic conditions or compromised immune systems due to disability are at higher risk of death due to COVID-19. Chronic conditions may be non-communicable diseases such as coronary artery disease, chronic obstructive pulmonary diseas (COPD), and diabetes or disabilities. If the decedent had existing chronic conditions, such as these, they should be reported in Part 2 of the medical certificate of cause of death.
WHO openly admits that people with underlying health problems are at a greater risk of death. This isn’t exactly revolutionary. It does make one ask why it’s necessary to drive up fear like this.
5. Global Surveillance For Infection January 2020
Recommendations for laboratory testing
Any suspected case should be tested. However, depending on the intensity of the transmission, the number of cases and the laboratory capacity, only a randomly selected sample of the suspect cases may be tested.
.
If resources allow, testing may be done more broadly (for instance through sentinel surveillance) to better assess the full extent of the circulation of the virus.
.
Based on clinical judgment, clinicians may opt to order a test in a patient not strictly meeting the case definition, such as for a cluster of acute respiratory illness among healthcare workers.
This of course raises an interesting question: how many of these samples are actually tested? How many are collected and just sit on a shelf somewhere?
If initial testing is negative in a patient who is strongly suspected to have novel coronavirus infection, the patient should be resampled and specimens collected from multiple
respiratory tract sites (nose, sputum, endotracheal aspirate). Additional specimen may be collected such as blood, urine, and stool, to monitor the presence of virus of and shedding of virus from different body compartments.
Doesn’t speak too highly of the test, if the recommendation of a negative result is to retest, based on suspicions. Of course, “strongly suspected” is entirely subjective.
Detecting the presence of a virus being shed? Isn’t that consistent with the claim that viruses are really exosomes, excreted from the body?
6. Global Surveillance For Infection March 2020
Case definitions for surveillance
Case and contact definitions are based on the current available information and are regularly revised as new information accumulates. Countries may need to adapt case definitions depending on their local epidemiological situation and other factors. All countries are encouraged to publish definitions used online and in regular situation reports, and to document periodic updates to definitions which may affect the interpretation of surveillance data.
Probable case
A. A suspect case for whom testing for the COVID-19 virus is inconclusive.
OR
B. A suspect case for whom testing could not be performed for any reason.
The World Health Organization actually suggests that countries can make up their own definitions of what a case is. So much for consistency. Also, inconclusive tests, or cases where tests aren’t performed can be written up as “probable” cases.
7. Global Surveillance For Infection May 2020
Purpose of the document
This document provides an overview of surveillance strategies that Member States should consider as part of
comprehensive national surveillance for COVID-19. This document emphasises the need to adapt and reinforce existing national systems where appropriate and to scale-up surveillance capacities as needed.
Most countries will need to significantly strengthen surveillance capacities to rapidly identify cases of COVID‑19, follow-up their contacts, and to monitor disease trends over time. Comprehensive national surveillance for COVID-19 will require the adaptation and reinforcement of existing national systems where appropriate and the scale-up of additional surveillance capacities as needed. Digital technologies for rapid reporting, data management, and analysis will be helpful. Robust comprehensive surveillance once in place, should be maintained even in areas where there are few or no cases; it is critical that new cases and clusters of COVID-19 are detected rapidly and before widespread disease transmission occurs. Ongoing surveillance for COVID-19 is also important to understand longer-term trends in the disease and the evolution of the virus.
Individuals in the community
Individuals in the community can play an important role in the surveillance of COVID-19. Where possible, individuals who have signs and symptoms of COVID-19 should be able to access testing at the primary care level. Where testing at the primary level is not possible, community-based surveillance, whereby the community participates monitors and reports health events to local authorities, may be helpful for identifying clusters of COVID-19.
Participation in contact tracing and cluster investigations are other important ways in which individuals and communities contribute to the surveillance of COVID-19. Contact tracing is the identification of all persons who may have had contact with an individual with COVID-19. By following such contacts daily for up to 14 days since they had contact with the source case, it is possible to identify individuals who are at high risk of being infectious and/or ill and to isolate them before they transmit the infection to others. Contact tracing can be combined with door-to-door case-finding or systematic testing in closed settings, such as residential facilities, or with routine testing for occupational groups. See Contact tracing guidelines for COVID-19.
This document gives plenty of advice on how to go about doing contact tracing, and these procedures are being used. But it has to be said that the means that they classify cases and deaths throws everything into doubt. A cynic may just wonder if this is just to set up a surveillance apparatus.
8. Global Surveillance For Infection August 2020
[Page 2]
Probable COVID-19 case:
A. A patient who meets clinical criteria above AND is a contact of a probable or confirmed case, or epidemiologically linked to a cluster of cases which has had at least one confirmed case identified within that cluster.
B. A suspected case (described above) with chest imaging showing findings suggestive of COVID-19 disease*
* Typical chest imaging findings suggestive of COVID-19 include the following (Manna 2020):
• chest radiography: hazy opacities, often rounded in morphology, with peripheral and lower lung distribution
• chest CT: multiple bilateral ground glass opacities, often rounded in morphology, with peripheral and lower lung
distribution
• lung ultrasound: thickened pleural lines, B lines (multifocal, discrete, or confluent), consolidative patterns with or without air bronchograms.
C. A person with recent onset of anosmia (loss of smell) or ageusia (loss of taste) in the absence of any other identified cause.
D. Death, not otherwise explained, in an adult with respiratory distress preceding death AND who was a contact of a probable or confirmed case or epidemiologically linked to a cluster which has had at least one confirmed case identified within that cluster.
[Page 3]
3. Definition of death due to COVID-19
A COVID-19 death is defined for surveillance purposes as a death resulting from a clinically compatible illness in a probable or confirmed COVID-19 case, unless there is a clear alternative cause of death that cannot be related to COVID-19 disease (e.g. trauma). There should be no period of complete recovery between the illness and death.
4. Recommendations for laboratory testing
Suspected and probable cases should be investigated for the presence of SARS-CoV-2 virus according to WHO guidance on Diagnostic testing for SARS-CoV-2. While recommended response activities are largely the same for probable and confirmed cases, testing of probable cases, where resources allow, is still useful since it can exclude cases and reduce the burden required for isolation and contact tracing.
.
Depending on the intensity of the transmission in a specific location, the number of cases and the laboratory capacity, a subset of suspected or probable cases can be prioritized for testing. WHO has provided recommendations on how to prioritize persons to be tested during community transmission in Laboratory testing strategy recommendations for COVID-19.
So, no tests actually have to be performed in order to consider a person a “probable case”. And if a person who had contact with a “probable case” dies, that person can also be considered one, if there was some respiratory issue.
Death has to be “clinically compatible” with how they believe this illness works. As long as there are no obvious signs (like bullet wounds), a case can be written up as a Covid-19 death. Such a system seems ripe for abuse, especially considering the political agenda being played out here.
9. Global Surveillance For Infection Dec. 2020
[Page 2]
Probable COVID-19 case:
A. A patient who meets clinical criteria above AND is a contact of a probable or confirmed case, or epidemiologically linked to a cluster of cases which has had at least one confirmed case identified within that cluster.
B. A suspected case (described above) with chest imaging showing findings suggestive of COVID-19 disease*
* Typical chest imaging findings suggestive of COVID-19 include the following (Manna 2020):
• chest radiography: hazy opacities, often rounded in morphology, with peripheral and lower lung distribution
• chest CT: multiple bilateral ground glass opacities, often rounded in morphology, with peripheral and lower lung
distribution
• lung ultrasound: thickened pleural lines, B lines (multifocal, discrete, or confluent), consolidative patterns with or without air bronchograms.
C. A person with recent onset of anosmia (loss of smell) or ageusia (loss of taste) in the absence of any other identified cause.
D. Death, not otherwise explained, in an adult with respiratory distress preceding death AND who was a contact of a probable or confirmed case or epidemiologically linked to a cluster which has had at least one confirmed case identified within that cluster.
[Page 3]
3. Definition of death due to COVID-19
A COVID-19 death is defined for surveillance purposes as a death resulting from a clinically compatible illness in a probable or confirmed COVID-19 case, unless there is a clear alternative cause of death that cannot be related to COVID-19 disease (e.g. trauma). There should be no period of complete recovery between the illness and death.
4. Recommendations for laboratory testing
Suspected and probable cases should be investigated for the presence of SARS-CoV-2 virus according to WHO guidance on Diagnostic testing for SARS-CoV-2. While recommended response activities are largely the same for probable and confirmed cases, testing of probable cases, where resources allow, is still useful since it can exclude cases and reduce the burden required for isolation and contact tracing.
.
Depending on the intensity of the transmission in a specific location, the number of cases and the laboratory capacity, a subset of suspected or probable cases can be prioritized for testing. WHO has provided recommendations on how to prioritize persons to be tested during community transmission in Laboratory testing strategy recommendations for COVID-19.
The definition of a “Death due to Covid-19” is still the same, and can include people where no test was performed, as long the illness is compatible with what is expected.
It’s interesting that despite all these samples being taken, it seems that the bulk aren’t being tested. By contrast, it seems to be random samples, unless a problem is detected.
10. Is This About Establishing Police State?
What is really going on here? Is all of this contact tracing just an underhanded method of establishing the structure of a surveillance state across the globe? This disease clearly can’t be as deadly as it’s made out to be, if Governments have to artificially inflate the numbers.
Virus likely has never been isolated
Modelling compromised: Imperial College London
Modelling compromised: London School of Hygiene & Tropical Medicine
Modelling compromised: Vaccine Impact Modelling Consortium
No basis for the PCR tests that are used
No evidence that masks actually work as advertised
No evidence, still that masks do anything
No basis for 2 meter “social distancing”
Lobbying behind “non-essential” business determination
No science to what Bonnie Henry does
Politicians and media talking heads are always harping on about “following the science”. Guess what? There isn’t any pushing this so-called pandemic.
