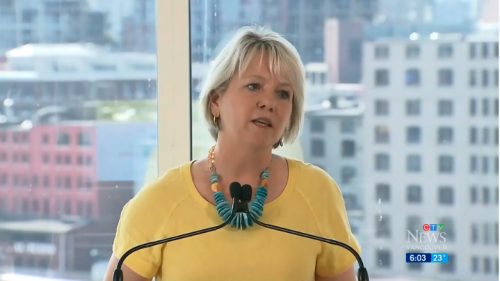
Apparently, Bonnie Henry is going to be pressuring people to take the experimental “vaccine”, but will get getting private businesses to do the dirty work.
Health Minister, Adrian Dix, didn’t have much to say in a meaningful sense. After all, his education in history and political science didn’t really prepare him for the role.
People in B.C. may be a bit confused. After all, the Protective Measures (COVID-19) Order was repealed on June 28, 2021. Also, the State of Emergency from March 2020 was formally cancelled.
Guess we can forget about a peaceful life in B.C. Will there also be emergency measures reintroduced at some point? After all, there are still plenty of people who see through this act.
From the looks of things, it seems that the B.C. Government won’t mandate it. However, they will encourage businesses to impose such a policy. Now, will they be subsidized to enforce such rules? Will there be extra perks for places that do?
Many people know about the 2015 Ontario Labour Arbitration which the ONA fought against a mandatory VOM “vaccinate-or-mask” policy. What less people know is that Bonnie Henry was an expert witness in that case.
Case: Sault Area Hospital and Ontario Nurses’ Association, 2015 CanLII 55643 (ON LA)
No joke. Less than a decade ago, Bonnie was telling an Ontario Hearing that there was no real evidence that masks or vaccines worked against influenza. Since then, she has changed her tune, and says something quite different. Although the ruling is readily available, there don’t appear to be transcripts.
134. Dr. Henry agreed with this observation by Dr. Skowronski and Dr. Patrick who are her colleagues at the British Columbia Centre for Disease Control:
.
I do agree, as we’ve discussed earlier, influenza is mostly transmitted in the community and we don’t have data on the difference between vaccinated and unvaccinated healthcare workers and individual transmission events…in healthcare settings.
.
135. Dr. Henry agreed that no VOM policy would influence influenza in the community. Dr. McGeer denied that she had used or recommended the use of community burden in the assessment of development of such a policy.
So there is no data on any differences between vaccinated and unvaccinated health care workers. Yet these people are still arguing for VOM (vaccine or mask).
145. In her Report Dr. Henry also referred to observational studies as supporting the data she said was derived from the RCTs but acknowledged that these studies related to long term care and not acute care settings. She was cross-examined at length concerning the studies referenced in this section of her Report, some that dealt with other closed community settings, and agreed that they were “clearly not referring to a healthcare setting”.
.
146. Witness commentary concerning the observational/experimental studies relied upon in the McGeer/Henry Reports is set out in Appendix A to this Award. I conclude from a review of these studies, and the expert witness commentary, that they do not disclose a consistent position. They address a wide range of issues in a wide range of settings. Some are not supportive of the OHA/SAH experts’ claim. Some provide weak support at best. Some have nothing to do with the issue in question. Some have acknowledged study design limitations.
Evidence introduced by Bonnie Henry was for long term care centers, not health care settings, so this apples and oranges. There is also weak or irrelevant evidence argued.
160. In direct examination Dr. Henry stated that the pre-symptomatic period was “clearly not the most infectious period but we do know that it happens”.[203] She also agreed in cross-examination that transmission required an element of proximity and a sufficient amount of live replicating virus.
.
161. At another point, the following series of questions and answers ensued during Dr. Henry’s cross-examination:
.
Q. With respect to transmission while asymptomatic, and I want to deal with your authorities with respect to that, would you agree with me that there is scant evidence to support that virus shedding of influenza actually leads to effective transmission of the disease before somebody becomes symptomatic?
.
A. I think we talked about that yesterday, that there is some evidence that people shed prior to being symptomatic, and there is some evidence of transmission, that leading to transmission, but I absolutely agree that that is not the highest time when shedding and transmission can occur.
.
Q. So were you—I put it to you that there’s scant evidence, and that was Dr. De Serres’ evidence, so—but that there’s very little evidence about that, do you agree?
.
A. There is—as we talked about yesterday, there is not a lot of evidence around these pieces, I agree.
.
Q. And clearly transmission risk is greatest when you’re symptomatic, when you’re able to cough or sneeze?
.
A. Transmission risk is greatest, as we’ve said, when you’re symptomatic, especially in the first day or two of symptom onset
Not a lot of evidence regarding risks of transmission. Yes, this is 2015, but it coming straight from BCPHO Bonnie Henry.
177. Dr. McGeer and Dr. Henry presented the position of the OHA and the Hospital based upon their understanding of the relevant literature. Neither of them asserted that they had particular expertise with respect to masks or had conducted studies testing masks.
So, no actual expertise of research. Bonnie Henry just read what was available. And this is the Provincial Health Officer of British Columbia.
184. In her pre-hearing Report Dr. Henry responded to a request that she discuss the evidence that masks protect patients from influenza this way:
.
There is good evidence that surgical masks reduce the concentration of influenza virus expelled into the ambient air (a 3.4 fold overall reduction in a recent study) when they are worn by someone shedding influenza virus. There is also evidence that surgical masks reduce exposure to influenza in experimental conditions.
.
Clinical studies have also suggested that masks, in association with hand hygiene, may have some impact on decreasing transmission of influenza infection. These studies are not definitive as they all had limitations. The household studies are limited by the fact that mask wearing did not start until influenza had been diagnosed and the patient/household was enrolled in the study, such that influenza may have been transmitted prior to enrollment. A study in student residences is limited by the fact that participants wore their mask for only approximately 5 hours per day. Two systematic reviews of the cumulative studies conclude that there is evidence to support that wearing of masks or respirators during illness protects others, and a very limited amount of data to support the use of masks or respirators to prevent becoming infected
.
In summary, there is evidence supporting the use of wearing of masks to reduce transmission of influenza from health care workers to patients. It is not conclusive, and not of the quality of evidence that supports influenza vaccination. Based on current evidence, patient safety would be best ensured by requiring healthcare providers to be vaccinated if they provide care during periods of influenza activity. However, if healthcare workers are unvaccinated, wearing masks almost certainly provides some degree of protection to their patients.
Bonnie Henry keeps hedging her answers. Yes, there is protection, but there are issues with the studies, and the evidence isn’t conclusive. She also takes the position that vaccinating everyone in health care settings would be prefereable.
219. Dr. Henry answered the ‘why not mask everyone’ question this way:
.
It is [influenza vaccination] by far, not perfect and it needs to be improved, but it reduces our risk from a hundred percent where we have no protection to somewhat lower. And there’s nothing that I’ve found that shows there’s an incremental benefit of adding a mask to that reduced risk…..there’s no data that shows me that if we do our best to reduce that incremental risk, the risk of influenza, that adding a mask to that will provide any benefit. But if we don’t have any protection then there might be some benefit when we know our risk is greater.
.
When we look at individual strains circulating and what’s happening, I think we need it to be consistent with the fact that there was nothing that gave us support that providing a mask to everybody all the time was going to give us any additional benefit over putting in place the other measures that we have for the policy. It’s a tough one. You know, it varies by season.[320]
.
It is a challenging issue and we’ve wrestled with it. I’m not a huge fan of the masking piece. I think it was felt to be a reasonable alternative where there was a need to do—to feel that we were doing the best we can to try and reduce risk.
.
I tried to be quite clear in my report that the evidence to support masking is not as great and it is certainly not as good a measure
Bonnie Henry admits no strong evidence to support maskings. However, that was 2015, and apparently the science has changed completely since then. Or perhaps just the politics.
In any event, she seems content pushing experimental, unapproved “vaccines” on the public. Of course, the manufacturers are indemnified against liability.
Even within the last year her view on masks changed considerably. It’s a good thing people document and archive these inconsistencies. Kudos to whoever made this compilation. Otherwise, people like Bonnie Henry, Adrian Dix, John Horgan and Mike Farnworth would be more easily able to rewrite history, and conceal their deceptions
Don’t worry! Action4Canada will be filing their lawsuit any day now, and that will save us! They are just one fundraiser away from being almost ready to start. (Yes, this is sarcasm.)
(1) https://bc.ctvnews.ca/not-vaccinated-against-covid-19-b-c-s-health-officials-say-there-will-be-consequences-1.5525139
(2) https://www.bclaws.gov.bc.ca/civix/document/id/mo/mo/m0275_2021?fbclid=IwAR309l-HdQCrEdBaF6q2dUMwr5CbevxjJ94CweOLK-VUSBx7bE-weX725KE
(3) https://www2.gov.bc.ca/assets/gov/public-safety-and-emergency-services/emergency-preparedness-response-recovery/embc/reports/speaker/621140-letter_to_the_speaker-protective_measures-m273.pdf
(4) https://www.canlii.org/en/on/onla/doc/2015/2015canlii62106/2015canlii62106.pdf
(5) 2015.ontario.nurses.association.mask.ruling
(6) https://www.canlii.org/en/on/onla/doc/2015/2015canlii62106/2015canlii62106.html
(7) https://www.canlii.org/en/on/onla/doc/2016/2016canlii76496/2016canlii76496.html
(8) https://canucklaw.ca/wp-content/uploads/2020/08/2018.ontario.college.of_.nurses.mask_.ruling.pdf

This is one Canadian who…if the vaccine passport goes thru…will never buy B.C. goods, nor will I go into BC for any reason. Love your wine, but from now on it’s U.S.A. all the way
It’s very hard to read the reams of mumbo jumbo, such as that looked at here, and to realize that those practitioners of voodoo have authority and can push citizens around at the behest of unelected, and deep-pocketed, powerful special interests.
It’s done that way on purpose, so you don’t see the bigger picture.