https://canucklaw.ca/wp-content/uploads/2021/01/BC-COVID19_InterpretingTesting_Results_NAT_PCR.pdf
http://www.bccdc.ca/Health-Professionals-Site/Documents/COVID19_InterpretingTesting_Results_NAT_PCR.pdf
https://www.cpsbc.ca/for-physicians/college-connector/2020-V08-02/04
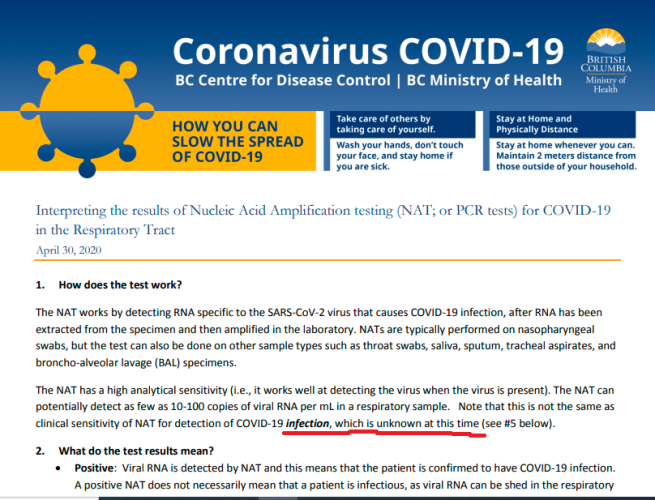
1. How does the test work?
The NAT works by detecting RNA specific to the SARS-CoV-2 virus that causes COVID-19 infection, after RNA has been extracted from the specimen and then amplified in the laboratory. NATs are typically performed on nasopharyngeal swabs, but the test can also be done on other sample types such as throat swabs, saliva, sputum, tracheal aspirates, and broncho-alveolar lavage (BAL) specimens.
.
The NAT has a high analytical sensitivity (i.e., it works well at detecting the virus when the virus is present). The NAT can potentially detect as few as 10-100 copies of viral RNA per mL in a respiratory sample. Note that this is not the same as clinical sensitivity of NAT for detection of COVID-19 infection, which is unknown at this time (see #5 below)
2. What do the test results mean?
Positive: Viral RNA is detected by NAT and this means that the patient is confirmed to have COVID-19 infection.
A positive NAT does not necessarily mean that a patient is infectious, as viral RNA can be shed in the respiratory tract for weeks but cultivatable (live) virus is typically not detected beyond 8 to 10 days after symptom onset.
Negative: Viral RNA is not detected in the sample. However, a negative test result does not totally rule out COVID-19 infection as there may be reasons beyond test performance that can result in a lack of RNA detection in patients with COVID-19 infection (false negatives; see below).
Indeterminate: The NAT result is outside the validated range of the test (i.e., RNA concentration is below the
limit of detection, or a non-specific reaction), or this might occur when the sample collected is of poor quality
(i.e., does not contain a sufficient amount of human cells). Indeterminate results do not rule in or rule out infection.
.
Overall, clinical judgement remains important in determining the implications of NAT test results, and whether a repeat test is indicated for negative or indeterminate results (for example, if the patient’s recent exposures or clinical presentation suggest COVID-19 infection is likely, diagnostic tests for other respiratory pathogens remain negative, or there is worsening of symptoms). For clinical guidance including testing and specimen collection, please refer to COVID-19 testing guidelines for British Columbia.
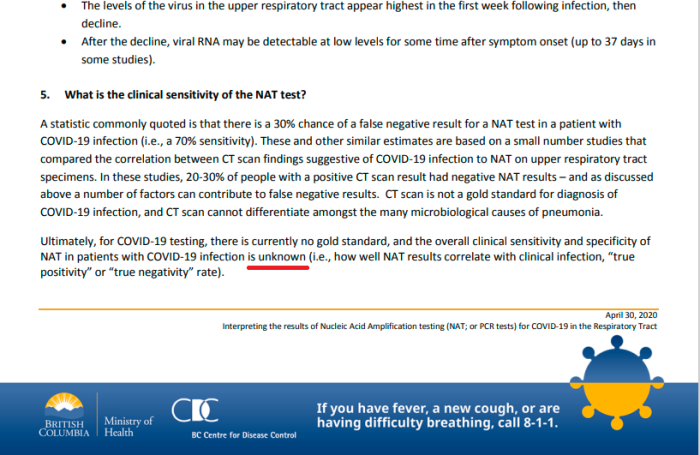
5. What is the clinical sensitivity of the NAT test?
A statistic commonly quoted is that there is a 30% chance of a false negative result for a NAT test in a patient with COVID-19 infection (i.e., a 70% sensitivity). These and other similar estimates are based on a small number studies that compared the correlation between CT scan findings suggestive of COVID-19 infection to NAT on upper respiratory tract specimens. In these studies, 20-30% of people with a positive CT scan result had negative NAT results – and as discussed above a number of factors can contribute to false negative results. CT scan is not a gold standard for diagnosis of COVID-19 infection, and CT scan cannot differentiate amongst the many microbiological causes of pneumonia.
.
Ultimately, for COVID-19 testing, there is currently no gold standard, and the overall clinical sensitivity and specificity of NAT in patients with COVID-19 infection is unknown (i.e., how well NAT results correlate with clinical infection, “true positivity” or “true negativity” rate).
Some points to take away
-Detecing RNA does not mean infection
-Error rate in infection detection is unknown.
-Positive test is meaningless
-Negative test is meaningless
-Can’t distinguish with many microbial causes of pneumonia
-30% false negative rate just a “commonly quoted statistic”
-Actual accuracy rate unknown
As for the “deaths due to Covid” perhaps check out the guidelines passed down College of Physicians and Surgeons of British Columbia:
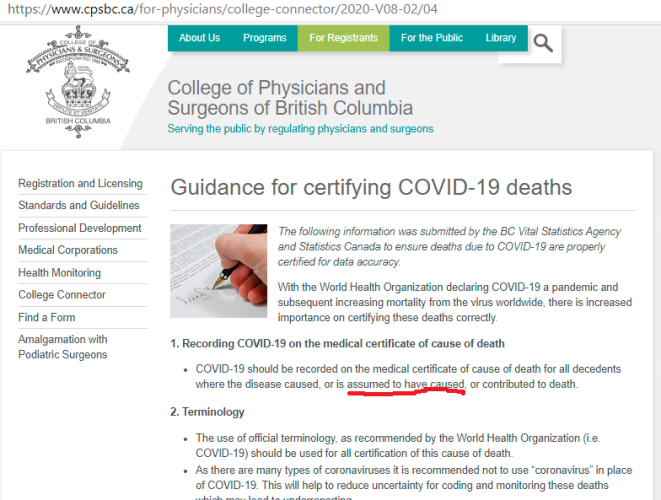
1. Recording COVID-19 on the medical certificate of cause of death
COVID-19 should be recorded on the medical certificate of cause of death for all decedents where the disease caused, or is assumed to have caused, or contributed to death.
In other words, just make it up.
Discover more from Canuck Law
Subscribe to get the latest posts sent to your email.

Excellent News!
Well Done!